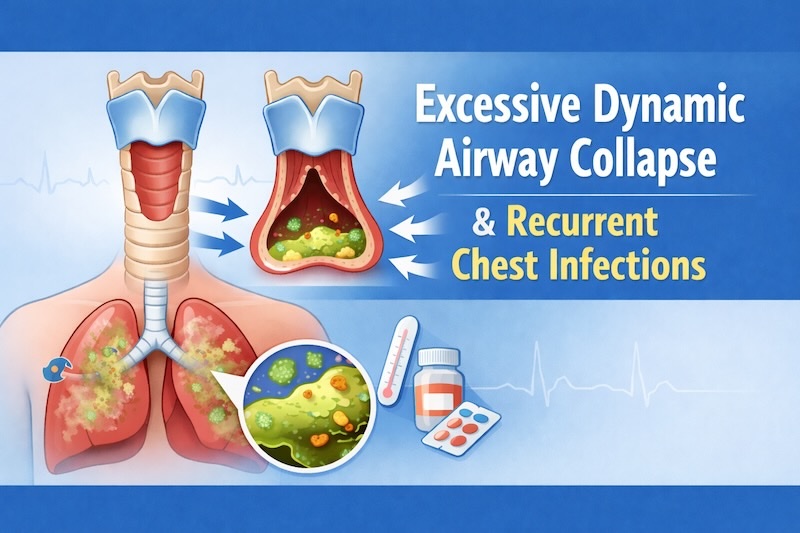
Excessive dynamic airway collapse (EDAC) can drive recurrent chest infections, stubborn cough, and breathlessness. It happens when the back wall of the windpipe and main bronchi buckle too much on breathing out, narrowing the airway by at least 50%. That narrowing traps mucus, impairs clearance, and invites infection. Understanding EDAC and how it differs from tracheobronchomalacia (TBM) is key to breaking the cycle of infections and flare-ups.
What is EDAC (and how is it different from TBM)?
EDAC and TBM sit under the umbrella term “expiratory central airway collapse” (ECAC). In EDAC, the cartilage rings are intact, but the posterior, membranous wall is lax and bows inward during expiration. In TBM, the cartilaginous wall is weakened or soft. Both cause excessive expiratory narrowing, but the structural targets differ and that matters for treatment planning.
Why EDAC leads to recurrent chest infections
When the central airways collapse on exhalation, airflow stalls and secretions pool. Thick, static mucus is hard to clear and becomes a growth medium for bacteria and viruses. People with EDAC then experience a cycle of wet cough, wheeze, breathlessness, and repeated chest infections that can mimic or complicate asthma and COPD. Managing mucus and stabilising the airway reduce infection risk.
Who is at risk of excessive dynamic airway collapse?
EDAC is increasingly recognised in adults with chronic cough or breathlessness that seems “out of proportion” to spirometry. It can occur alongside or be mistaken for asthma or COPD. Other contributors include recurrent infections, prolonged airway inflammation, obesity, gastro-oesophageal reflux, and prior airway trauma or surgery. In children, related malacia may be congenital, while in adults it is often acquired.
Common symptoms of excessive dynamic airway collapse
- Persistent, often barking or brassy cough
- Noisy breathing or wheeze, worse on exertion
- Breathlessness that improves when leaning forward
- Trouble clearing phlegm; frequent chest infections
- Voice changes; occasionally dizziness or syncope with coughing fits
Symptoms may fluctuate day to day, which is one reason EDAC is under-diagnosed.
How EDAC is diagnosed
Start with suspicion. Normal spirometry doesn’t rule it out. Flattening of the expiratory limb on a flow–volume loop can hint at large airway collapse but is neither sensitive nor specific.
Dynamic expiratory CT (DACT). Low-dose CT acquired during forced expiration can show the degree and pattern of collapse. Across studies, dynamic CT demonstrates high diagnostic performance and correlates well with bronchoscopic findings, although exact sensitivity varies by protocol and population. It is non-invasive and widely available, making it a strong first-line test.
Flexible bronchoscopy with forced expiration. This remains the reference standard. It allows direct visualisation of airway behaviour, classification of collapse (EDAC vs TBM vs mixed), and assessment of the extent (trachea, main bronchi). Dynamic bronchoscopy is especially valuable when planning intervention. Many centres consider >50% expiratory narrowing diagnostic, but severity scales and thresholds continue to evolve.
Four-dimensional CT and advanced imaging. Emerging 4D CT techniques capture airway motion over time and may refine grading and treatment decisions, though availability is limited.
Why infections keep coming back—and how to break the cycle
Airway collapse blocks effective expiratory flow and hinders mucociliary clearance. Mucus lingers, becomes more viscous, and fosters bacterial overgrowth. Each infection inflames the airway further, potentially worsening collapse—a self-perpetuating loop. Management therefore targets both the collapsing airway and the mucus burden:
- Stabilise the airway during expiration (e.g., positive pressure, splinting, surgery in selected cases).
- Improve mucus clearance (e.g., airway clearance physiotherapy and devices).
- Reduce contributors (e.g., treat reflux, optimise asthma/COPD therapy, weight management).
Treatment options for EDAC
Optimising underlying conditions and triggers
Treat coexisting asthma, COPD, chronic rhinosinusitis, and reflux. Vaccinate against influenza and pneumococcus per national guidance. Each step reduces exacerbations and infectious risk while you address the airway mechanics.
Airway clearance physiotherapy
Targeted techniques—active cycle of breathing, autogenic drainage, huff coughing, and use of devices such as oscillatory PEP—help move secretions from the central airways. NHS physiotherapy guidance emphasises tailored programmes, regular practice, and hydration. Many patients notice fewer infections once an effective routine is in place.
Positive airway pressure (PAP: CPAP/BiPAP)
PAP “splints” the central airway open during expiration, improving flow and secretion clearance. Observational cohorts and case reports show symptom and quality-of-life gains in selected patients, with reduction in cough and infections; however, response varies and formal guidelines are still developing. Pressure titration is important, and some patients need nocturnal use only; others benefit during exertion or physiotherapy.
Endoscopic therapies
Short-term silicone or metallic stents can assess whether mechanical stabilisation relieves symptoms (“stent trial”). Long-term stenting may help selected non-surgical candidates but carries risks (migration, mucus plugging, granulation tissue). Decision-making should sit with an experienced interventional team.
Surgical tracheobronchoplasty (TBP)
In severe, diffuse EDAC or TBM with persistent symptoms despite optimised conservative care, TBP reinforces the posterior membranous wall with a mesh to prevent dynamic collapse. Contemporary series suggest meaningful improvements in dyspnoea, cough, and function in appropriately selected patients, though surgery is specialised and not suitable for everyone. Shared decision-making and centre experience matter.
Living with EDAC: practical tips to cut infection risk
- Master your airway clearance routine. Do it daily and increase during colds. Pair sessions with warm drinks or saline nebulisers if prescribed.
- Use positive pressure strategically. Many find PAP just before and during physiotherapy improves mucus mobilisation. Work with your clinic to set pressures that stabilise but don’t over-inflate.
- Optimise inhaled therapy if you also have asthma/COPD. The goal is calm, non-inflamed airways that collapse less and clear better.
- Treat reflux and post-nasal drip. Micro-aspiration and throat clearing can aggravate cough and airway irritation.
- Stay up to date with vaccines and seek early advice for worsening chest symptoms.
- Know your red flags. High fever, chest pain, sudden breathlessness, or coughing up blood warrant urgent assessment.
What to expect from care pathways
Because EDAC overlaps with more familiar diseases, many patients reach diagnosis after months or years. Ask to see a specialist, who understands the condition and can arrange a dynamic expiratory CT or bronchoscopy, if infections and cough persist despite standard care. Tertiary centres with interventional pulmonology, physiotherapy expertise and thoracic surgery offer comprehensive assessment, stent trials when appropriate, and surgical opinions. With the right combination of clearance techniques, PAP, and (for some) intervention, many people reduce infections and regain confidence in daily life.
Key takeaways
- EDAC is a mechanical cause of cough and recurrent chest infections due to excessive expiratory narrowing of the central airways.
- Dynamic expiratory CT and bronchoscopy confirm the diagnosis and guide therapy.
- Airway clearance and positive pressure are first-line mainstays, with stents or surgery for selected patients.
- Treat comorbidities and triggers to reduce inflammation and break the infection cycle.
FAQs
1) Is EDAC the same as tracheobronchomalacia?
No. Both cause expiratory airway narrowing, but EDAC involves laxity of the posterior membrane with normal cartilage, while TBM reflects weakness of the cartilaginous wall. Management differs accordingly.
2) Can EDAC be missed on routine spirometry or a standard CT?
Yes. Spirometry can look “normal,” and a static (resting) CT may not show collapse. Dynamic expiratory CT and/or bronchoscopy are usually needed.
3) Will CPAP cure EDAC?
CPAP doesn’t cure the structural tendency to collapse, but it can splint the airway and improve symptoms, clearance, and infection frequency in selected patients. Response varies, and pressures should be individualised.
4) When is surgery considered?
If symptoms remain severe despite optimal medical and physiotherapy strategies, and a stent trial suggests benefit, specialists may discuss tracheobronchoplasty. Suitability depends on anatomy, extent of disease, and overall health.
5) Why do I keep getting chest infections?
Dynamic collapse traps mucus, which is fertile ground for bacteria and viruses. Clearance techniques plus airway stabilisation reduce pooling and infection risk.
GET IN TOUCH
Schedule a Visit with Dr Ricardo Jose
Disclaimer: The information provided in this article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your healthcare provider with any questions you may have regarding a medical condition or treatment
