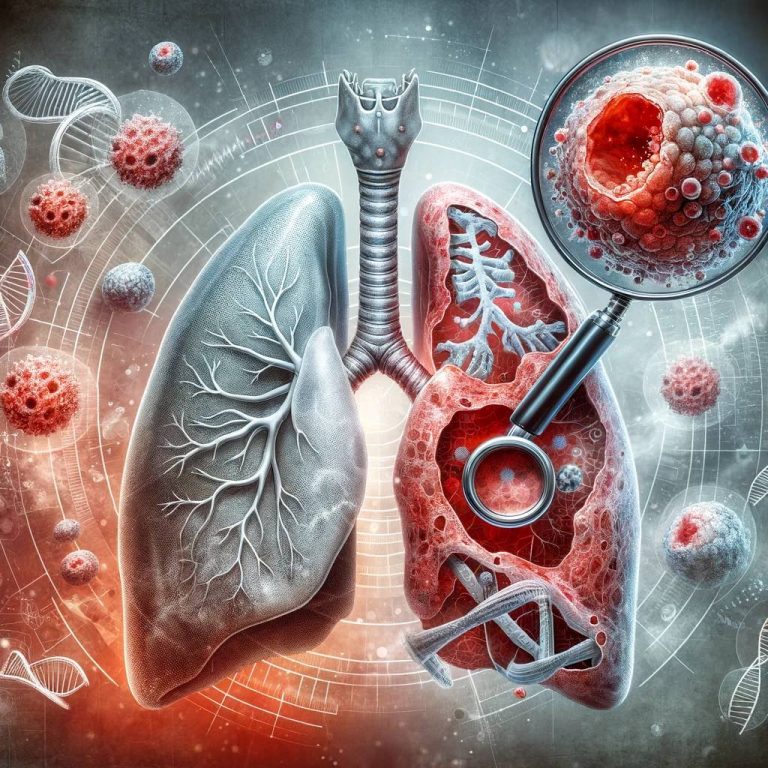
Lung cancer is the top cause of cancer-related deaths worldwide. It ranks as one of the most prevalent types of cancer among both men and women. This disease is most frequently diagnosed in individuals over 70 years of age, and it is rare in those under 40. A major challenge with lung cancer is that symptoms often manifest late in the disease’s progression, leading to a poor prognosis in advanced stages.
Lung cancer is a serious type of cancer because many people don’t experience symptoms until the disease is advanced and difficult to treat.
Symptoms usually include:
While smoking remains the primary risk factor for lung cancer, recent trends show a rising incidence of lung cancer among non-smokers. This shift highlights the importance of understanding other significant risk factors. These include exposure to asbestos and radon gases, the effects of second-hand smoke, and the potential impact of air pollution, particularly diesel exhaust fumes. Each of these factors can lead to genetic alterations in lung cells, paving the way for the development of lung cancer.
Moreover, family history plays a crucial role in lung cancer risk. Individuals with relatives who have had lung cancer are at a higher risk, often due to inherited genetic mutations. However, it’s important to note that this genetic predisposition accounts for a relatively small percentage of total lung cancer cases.

The diagnosis of lung cancer typically involves obtaining a tumour sample to identify cancer cells under a microscope. In instances where this isn’t feasible or necessary, a clinical diagnosis may be made by a multi-disciplinary cancer team.
Radiological imaging plays a crucial role when clinical history indicates possible lung cancer. Techniques like computed tomography (CT) scans are more sensitive than X-rays in detecting lung cancer. They provide detailed information about the tumour’s size, shape, and location, and can reveal other critical findings such as enlarged mediastinal or hilar lymph nodes, or the presence of metastasis in bones, adrenal glands, or liver.
Several methods are used for biopsies. These include endobronchial biopsies for visible endobronchial lesions, or CT-guided biopsies of the lung mass. For enlarged mediastinal or hilar lymph nodes, a transbronchial lymph node biopsy can be performed using endobronchial ultrasound. Additionally, ultrasound-guided biopsies are employed for sampling distant lymph nodes, such as those above the clavicle or in the neck.
Positron emission tomography (PET) combined with CT scans are instrumental in detecting cancer’s spread in the body, aiding in disease staging.
Given the poor prognosis associated with lung cancer, early detection is imperative. Lung cancer screening is recommended for individuals at high risk.
The treatment for lung cancer is determined by the disease stage and cancer type.
Small cell lung cancer typically requires systemic chemotherapy and radiotherapy. As the brain is a common site for distant metastasis, preventative cranial irradiation in limited stage small cell lung cancer significantly reduces brain metastasis risk and improves survival rates. However, due to its rapid spread, surgery is rarely an option, reserved only for a small minority of early-detected cases.
For tumours confined to a small area, surgical removal is possible. This could be a segmentectomy (removing a lung segment), a lobectomy (removing a lung lobe), or a pneumonectomy (removing the entire lung).
Localised small tumours may also be treated with stereotactic radiotherapy when surgery isn’t feasible.
In cases where lung cancer cannot be addressed with surgery or radiotherapy, options like systemic chemotherapy, targeted chemotherapy, or immunotherapy are considered, provided the patient is physically fit for such treatments.
Respiratory Medicine
Royal Brompton Hospital
Sydney Street
Chelsea
SW3 6NP