What is bronchiectasis?
Before discussing the treatment of bronchiectasis it is important to understand what bronchiectasis is and how it affects people. Bronchiectasis is a condition where there is abnormal dilation of the bronchi. There are several medical conditions that lead to this condition and need to be considered when treating people with bronchiectasis. However, in some people the cause of their bronchiectasis isn’t clear – this is known as idiopathic bronchiectasis. The most common cause of bronchiectasis is a previous chest infection, sometimes as far back as during childhood.
Bronchiectasis can result from congenital as well as acquired causes. Irrespective of the cause it leads to a vicious cycle of infection and inflammation. This causes further thickening of the bronchial walls and dilatation of the bronchi.
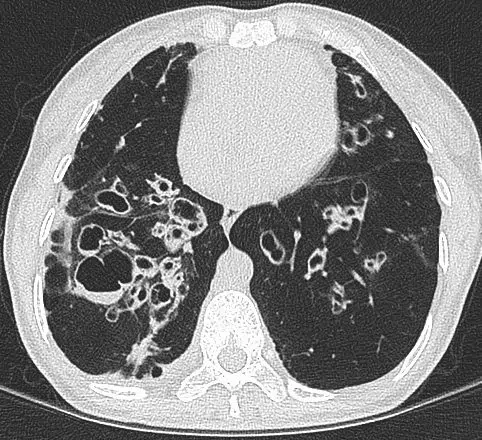
The inflamed airways produce excess mucus and chronic cough. Due to the structurally abnormal airways the phlegm may be hard to expectorate. The body’s natural defence mechanisms are impaired leading to recurrent chest infections. Individuals may experience episodes of increased production of phlegm, usually accompanied with a change in colour of the phlegm, worsening breathlessness, chest pain and fatigue over days. These episodes are exacerbations of the bronchiectasis. Medical treatment is needed to resolve this promptly as the attacks on the airways result in more damage. Additionally, exacerbations of bronchiectasis can lead to respiratory failure and cardiac complications such heart attacks. Because of the serious and frequently recurring nature of chest infections that have a significant negative impact on quality of life, people suffering with bronchiectasis require lifelong medical support from a specialist respiratory doctor.
Treatment and management of bronchiectasis
Treatment plans may differ depending on the cause of the bronchiectasis but in general they focus on long term improvement of symptoms and quality of life. Treatment plans are altered depending on how the individual’s situation changes over time. Unfortunately, there is no cure to reverse the structural lung disease. However, good management can attenuate progression and reduce the frequency of exacerbations.
The treatment plans also depend on the severity of the bronchiectasis, frequency of exacerbations and symptoms. Treatments range from chest physiotherapy to the use of mucolytics, antibiotics and anti-inflammatory agents. Treatment of associated infections such as infections with moulds or non-tuberculosis mycobacteria is also important to control bronchiectasis progression and symptoms.
Chest physiotherapy
Chest physiotherapy is the mainstay of bronchiectasis treatment and must not be overlooked. Physiotherapy focuses on airway clearance – coughing out the mucus is important to drain the chest of infected mucus, helping to reduce inflammation, airway obstruction and mucus production. There are different techniques for this procedure and an expert chest physiotherapist can offer guidance to the best technique for everyone’s situation. Three of the commonest forms of airway clearance include the Active Cycle of Breathing Technique, which involve breathing control, chest expansion exercises and huff coughing; autogenic drainage which makes use of changes in breath volume and speed to expel mucus from the bronchi to larger airways; and use of adjuncts such as a Positive Expiratory Pressure mask to prevent early closure of the airways and help move the mucus up the airways. Nebulised hypertonic saline restores the liquid lining the airways and facilitates mucus clearance.
Antibiotics
More severe cases require high penetrance antibiotics that in some cases are administered intravenously. Importantly, in bronchiectasis the duration of antibiotic therapy is longer that the standard course often prescribed to treat chest infections. Furthermore, in cases of chronic bacterial colonisation with frequent exacerbations, prolonged courses of prophylactic oral or nebulised antibiotics are often needed. Your chest specialist will discuss with you which preventative strategy is likely to be best for your situation and monitor the longterm effects. Azithromycin is a commonly used preventative oral antibiotic. In addition to the antibacterial properties, azithromycin has anti-inflammatory properties and has been shown to reduce the frequency of bronchiectasis exacerbations and attenuate mucus production. When colonisation with gram-negative bacterial pathogens is of concern nebulised antibiotics are a good choice to suppress the number of pathogenic bacteria within the airways and reduce infections. Nebulised colomycin is usually the first choice but several other antibiotics can be nebulised depending on the identified pathogens and respiratory physicians with particular expertise in this area can advise. Some people may only need preventative treatments during the Winter month’s whilst others will require it all year round.
In recent years, interest in bronchiectasis has increased due to the recognition of a rising prevalence of this respiratory condition and the impact it has on the lives of those suffering with it. There are ongoing trials of new inhaled antibiotics, mucolytics, CFTR modulators and anti-inflammatory medications for the treatment and management of bronchiectasis.
Self-help tips
There are certain recommended practices that can help people manage bronchiectasis better. Some of these include:
1. Maintaining a healthy diet which is low in sodium, added sugars, saturated fats, and refined grains.
2. Staying well hydrated as water helps reduce the viscocity of mucus making it easier to expectorate.
3. Performing airway mucus clearance techniques daily.
4. Being proactive about taking inhaled or oral medications as prescribed.
5. Quit smoking if smoking, and avoiding second hand passive smoking as well.
6. Ensuring vaccinations (e.g. pneumococcal and influenza) are up to date.
Even while maintaining a healthy lifestyle, it is important to keep in mind that exacerbations of bronchiectasis can still recur and advice from your specialist is needed.
In summary, treating bronchiectasis requires expert consultation while certain healthy practices can have long term benefits or prevent the condition from worsening.particu

