Introduction to Mast Cell Activation Syndrome (MCAS)
Mast Cell Activation Syndrome (MCAS) is a disorder that arises from an abnormal release of mast cell mediators, potentially causing a plethora of symptoms that can disrupt daily life. In certain cases, these symptoms manifest in the respiratory system, with impacts that can vary in severity.
Symptoms of Mast Cell Activation Syndrome
MCAS often presents with an extensive range of symptoms, making it a complex condition to diagnose. These symptoms can involve multiple systems in the body, and they can fluctuate in both type and intensity. Common symptoms include fatigue, skin rashes (urticaria), abdominal pain, nausea, and diarrhoea. Additionally, patients often suffer from headaches, brain fog, gastro-oesophageal reflux and bone or muscle pain. However, here the focus will be on respiratory symptoms, which are a significant concern for many patients.
Respiratory Symptoms of MCAS
Patients with MCAS may exhibit various respiratory symptoms, including coughing, wheezing, chest tightness, and difficulty breathing, much like those seen in asthma. Breathing pattern dysfunction is a common feature. Postnasal drip, sinusitis, and nasal congestion are also frequently reported. These symptoms can significantly affect patients’ quality of life and lead to additional health complications if left untreated.
Impact of MCAS on Respiratory Infections
MCAS can potentially influence cellular immunity and the body’s response to infections, though the exact mechanisms are still under investigation. The role of mast cells in immunity is complex and multifaceted, contributing both to the initial recognition of pathogens and to the orchestration of the body’s immune response.
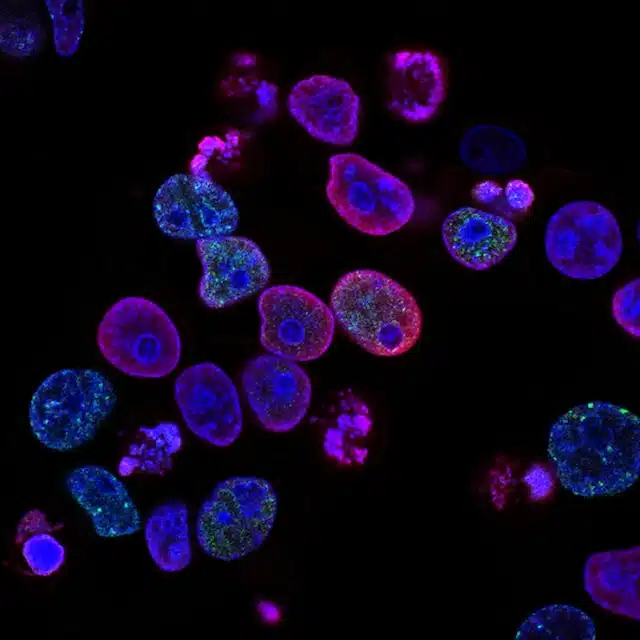
Mast cells, which are components of the body’s innate immune system, are known for their role in allergic reactions, but they are also involved in combating infections. They can recognise a broad array of pathogenic threats and respond by releasing various inflammatory mediators. Among these are histamine, proteases, cytokines, and chemokines, which can recruit and activate other immune cells, enhance blood vessel permeability, and stimulate mucus secretion. These actions help trap and remove pathogens and alert the rest of the immune system to the presence of an infection.
In MCAS, the mast cells are hyperactive, and they can degranulate and release these mediators inappropriately. This chronic, low-level inflammation may disrupt the balance of the immune system, possibly impairing its ability to respond effectively to pathogens.
MCAS can potentially exacerbate the severity of respiratory infections. The persistent inflammation and irritation caused by mast cell activation can weaken the respiratory system, making it more susceptible to infections. This susceptibility, in turn, may prolong recovery times and increase the severity of symptoms.
Diagnosis of Mast Cell Activation Syndrome
Diagnosing MCAS can be a complex process due to the broad array of possible symptoms and the overlap with other conditions. However, several criteria have been proposed, these include:
- Symptoms: The patient should have chronic or recurrent symptoms consistent with mast cell activation. These may include flushing, pruritus (itching), hives, nausea, vomiting, diarrhoea, abdominal pain, wheezing, shortness of breath, hypotension (low blood pressure), and others.
- Laboratory Evidence of Mast Cell Activation: Laboratory tests should show evidence of mast cell activation. This can include elevated levels of mediators released by mast cells, such as tryptase, histamine, or other mast cell-derived metabolites, like Leukotriene E4, prostaglandin D2 or its metabolite 11β-prostaglandin F2 alpha. It is important to note that these tests should be taken during a symptomatic episode to capture the increase in these markers.
- Response to Treatment: Symptoms should improve with treatment directed at blocking or stabilizing mast cells or inhibiting their mediators. For example, medications like H1 and H2 antihistamines, mast cell stabilisers, or leukotriene antagonists should provide symptom relief.
- Exclusion of Other Diseases: Other conditions that could account for the symptoms and laboratory findings must be ruled out. This could include allergic reactions, mastocytosis, and other immune disorders.
Treatment of Mast Cell Activation Syndrome
The treatment of MCAS is multifaceted and often includes medication, psychological support, lifestyle modifications, and diet changes.
Medication
Medication is a primary treatment method for MCAS and usually involves antihistamines and mast cell stabilisers. The former blocks the effects of histamine, which can help alleviate symptoms, while the latter prevent mast cells from releasing their mediators.
Psychological Support
As MCAS can be a distressing and life-altering condition, psychological support is a vital part of treatment. This may involve counselling or cognitive-behavioural therapy to help manage the emotional impact of living with the condition.
Lifestyle Modifications
Lifestyle modifications can also play a significant role in managing MCAS. These include regular exercise, adequate sleep, stress management, and avoiding known triggers of mast cell activation.
Exercise Recommendations in Mast Cell Activation Syndrome
Maintaining a healthy and active lifestyle is crucial for managing Mast Cell Activation Syndrome (MCAS). However, exercise can sometimes trigger symptoms in individuals with MCAS due to the release of stress hormones and heat-induced mast cell activation. Hence, the key to exercising with MCAS is balance – finding the right amount and type of exercise that benefits your health without exacerbating your symptoms.
Low-Intensity Exercises
In most cases, low to moderate intensity exercises are recommended. These exercises include:
- Walking: This is a gentle, low-impact activity that can be easily incorporated into your daily routine. Regular walks can improve cardiovascular health and overall fitness without causing undue stress on the body.
- Yoga: Yoga not only enhances flexibility and strength but also promotes mindfulness and stress relief, which can be beneficial for managing MCAS symptoms.
- Pilates: Similar to yoga, pilates focuses on strength, flexibility, and mindful movement, which can help improve overall wellness.
- Stretching: Regular stretching can maintain flexibility, improve circulation, and help prevent injuries, making it an excellent addition to your exercise regimen.
Water-based Exercises
Water-based exercises like swimming or water aerobics are often well-tolerated by individuals with MCAS. The water’s buoyancy reduces impact on the joints, while the cool water can prevent overheating, a common trigger for mast cell activation.
Tailoring Your Exercise Plan
While these are general guidelines, the most suitable exercise will depend on your individual situation, including your fitness level, severity of symptoms, and triggers. It is vital to listen to your body and adjust your exercise routine as needed.
For instance, if you find that intense workouts trigger your symptoms, it might be better to break up your exercise routine into shorter, more manageable sessions throughout the day. Additionally, consider exercising in a controlled environment where you can manage factors like temperature, to avoid heat-related triggers.
Diet
Dietary changes, such as adopting a low histamine diet, can also be beneficial. Foods high in histamine, including certain types of cheese, fermented foods, and alcohol, should be avoided.
Dietary management can play an essential role in controlling Mast Cell Activation Syndrome. Adopting a low histamine diet can help alleviate symptoms, given that histamine is one of the inflammatory mediators released by mast cells.
Remember, tolerance to histamine can vary greatly between individuals. Some people with MCAS may tolerate higher histamine foods better than others. Therefore, it can be helpful to keep a food diary to identify any specific dietary triggers. Always consult with a dietitian or healthcare provider when making significant changes to your diet. They can help you to develop a personalised meal plan that meets your nutritional needs while managing MCAS symptoms.
Differentiating Between MCAS and Mastocytosis
MCAS and mastocytosis, although similar, are distinct conditions. The former involves an abnormal release of mast cell mediators, while the latter involves an excessive number of mast cells in the body. The World Health Organisation’s evidence-based guidelines for the diagnosis of mastocytosis include a demonstration of an increased mast cell burden through a biopsy, something not usually seen in MCAS.
Criteria for the diagnosis of Mastocytosis
The diagnosis of systemic mastocytosis, a disorder characterized by an excessive accumulation of mast cells in one or more organ systems, is governed by a set of criteria established by the World Health Organization (WHO).
- Major Criterion: The presence of multifocal, dense infiltrates of mast cells (greater than or equal to 15 mast cells in aggregates) detected in sections of bone marrow and/or other extracutaneous organ(s).
- Minor Criteria:
- More than 25% of the mast cells in the infiltrate are spindle shaped or have atypical morphology, or, of all mast cells in bone marrow aspirate smears, more than 25% are immature or atypical.
- Detection of an activating point mutation at codon 816 of KIT in bone marrow, blood, or another extracutaneous organ.
- Mast cells in bone marrow, blood, or other extracutaneous organ express CD2 and/or CD25 in addition to normal mast cell markers.
- Serum total tryptase persistently exceeds 20 ng/mL (unless there is an associated clonal myeloid disorder, in which case this parameter is not valid).
For a diagnosis of systemic mastocytosis to be made, either the major criterion and one minor criterion, or three minor criteria must be met.
Disclaimer: The information provided in this article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your healthcare provider with any questions you may have regarding a medical condition or treatment.

