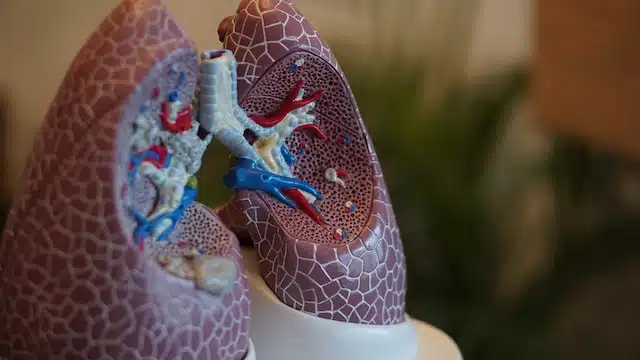
Defining Idiopathic Pulmonary Fibrosis (IPF)
IPF is a chronic and progressive lung disease.It is one the lung disease encompaseed in the term “Interstitial Lung Disease” The process, known as fibrosis, causes the lung tissues to thicken and stiffen, impeding normal respiratory function. The term ‘Idiopathic’ is used when the cause of this condition remains unknown.
The Pathology of IPF
The pathology of IPF initiates with an unidentified injury to the alveoli – the tiny air sacs within our lungs. In a normal scenario, an injury triggers a healing response. However, in IPF, this recovery mechanism is disrupted, leading to the overgrowth of fibrous, scar-like tissue. This tissue stiffness obstructs the smooth transfer of oxygen from the lungs to the bloodstream.
Recognising the Symptoms of IPF
The symptoms of IPF are often elusive and can be mistaken for common ailments or signs of ageing. These symptoms include:
- Chronic breathlessness, especially during physical activities.
- A consistent, dry cough.
- Persistent fatigue and weakness.
- Unintended weight loss.
- Discomfort in the chest.
Diagnosing IPF: Conditions to Exclude
Diagnosing IPF is a complex process. It necessitates ruling out other conditions with similar symptoms. These conditions include Chronic Obstructive Pulmonary Disease (COPD), asthma, heart diseases, and other non-idiopathic forms of pulmonary fibrosis such as:
- Sarcoidosis: A condition causing clumps of inflammatory cells, called granulomas, in the lungs or lymph nodes.
- Hypersensitivity Pneumonitis (HSP): A lung inflammation resulting from inhaling certain environmental substances.
- Asbestosis: A chronic lung disease caused by prolonged exposure to asbestos.
- Langerhans Cell Histiocytosis: A rare disorder leading to an overproduction of Langerhans cells, a type of white blood cell, affecting lung function.
To confirm an IPF diagnosis, respiratory specialists utilise a range of tests including Pulmonary Function Tests, High-resolution Computed Tomography (HRCT), Bronchoscopy and Lavage, and in some cases, a lung biopsy. A detailed review of the patient’s medical history and a comprehensive physical examination are also vital.
Monitoring in IPF: A Crucial Aspect
Monitoring in IPF is integral for managing the disease effectively. Regular follow-ups allow clinicians to track disease progression, manage symptoms, and adapt treatment strategies. The monitoring regimen typically includes:
- Periodic Lung Function Tests.
- The six-minute walk test to measure exercise tolerance.
- Serial imaging studies to observe the disease’s progression.
- Ongoing evaluation of symptoms and overall health.
Evidence-based Treatment of IPF
Currently, no definitive cure for IPF exists. However, treatments are available that slow disease progression and enhance patients’ quality of life:
- Antifibrotic medications: Pirfenidone and nintedanib can reduce lung tissue scarring, thus slowing disease progression.
- Oxygen therapy: This helps combat breathlessness and maintain optimal oxygen levels in the bloodstream to prevent pulmonary hypertension and strain on the right side of the heart.
- Pulmonary rehabilitation: This comprehensive programme includes exercise, education, and psychological support.
Antifibrotic Medications: Nintedanib and Pirfenidone
The centrepiece of IPF treatment revolves around two key antifibrotic medications, nintedanib and pirfenidone. Despite no cure being available for IPF, these medications have revolutionised disease management by slowing disease progression.
Understanding Nintedanib
Nintedanib, a type of drug known as a tyrosine kinase inhibitor, works by interfering with the pathways that cause lung scarring. By doing so, it slows down the rate of lung tissue thickening and stiffening.
Typically, the dosage for nintedanib is 150mg, taken orally twice daily with food. However, the dosage may be reduced to 100mg twice daily if the patient experiences adverse effects.
Some common side effects of nintedanib include:
- Diarrhoea: This is the most common side effect, which can often be managed with antidiarrhoeal medications.
- Nausea and vomiting: These side effects can be managed with the help of antiemetic drugs.
- Liver function abnormalities: Regular liver function tests are recommended to monitor these potential changes.
It’s worth noting that while these side effects can be inconvenient, they are generally manageable and the benefit of slowing the disease progression often outweighs these effects.
Decoding Pirfenidone
Pirfenidone works by decreasing the production of growth factors and procollagens I and II, proteins involved in the fibrotic process, hence slowing down the scarring of lung tissue.
The recommended dosage for pirfenidone varies, starting from a lower dose and gradually increasing to a maintenance dose. The maintenance dose is 801mg, taken orally three times a day with food.
Pirfenidone also carries some side effects, including:
- Gastrointestinal effects: Nausea, dyspepsia, vomiting, and anorexia can occur but are generally manageable with symptomatic treatment.
- Photosensitivity: This side effect can be mitigated by wearing sun-protective clothing and applying a broad-spectrum sunscreen.
- Fatigue and dizziness: These side effects can often be managed by adjusting the dose.
As with nintedanib, the side effects of pirfenidone are generally manageable, and the benefits of the drug often outweigh these side effects. Always discuss with your healthcare provider about any concerns you may have about side effects.
These antifibrotic medications signify a leap forward in the treatment of IPF. They serve as a testament to the relentless progress of medical science in our quest to manage this challenging disease.
Prognosis of IPF
The prognosis of IPF can vary widely among individuals. It is influenced by factors such as age, overall health, treatment response, and disease severity at the time of diagnosis. While IPF is progressive and often fatal, many patients can enjoy fulfilling lives for several years after diagnosis.
The Role of Lung Transplantation in IPF
In severe cases of IPF, a lung transplant may be considered. This complex surgery can significantly improve the patient’s quality of life and prolong survival. However, it comes with potential risks and necessitates a lifelong commitment to immunosuppressive medications.
Further guides
- NHS: Pulmonary fibrosis
- British Lung Foundation: Pulmonary fibrosis
- NIH: Idiopathic Pulmonary Fibrosis
- ATS: Idiopathic Pulmonary Fibrosis
- NICE: Idiopathic pulmonary fibrosis
GET IN TOUCH
Schedule a Visit
Disclaimer: The information provided in this article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your healthcare provider with any questions you may have regarding a medical condition or treatment.

