What is PCD?
Primary Ciliary Dyskinesia (PCD) is a rare congenital condition, primarily characterised by dysfunction in the cilia, the tiny hair-like structures that line our respiratory tract. These cilia serve as essential movers, propelling mucus and foreign particles out of our respiratory passages. Imagine a conveyor belt system in a large factory—when it breaks down, things get congested, leading to various complications.
Causes of Primary Ciliary Dyskinesia
Every individual carries a genetic code, a blueprint, handed down from their parents. This genetic hand-me-down process sometimes includes mutated genes that can lead to disorders like PCD.
Symptoms and Diagnosis
Recognising the Symptoms of PCD
Individuals with PCD often face chronic health challenges:
- Persistent cough: Due to mucus buildup, a chronic cough develops which can be distressing and fatiguing.
- Shortness of breath: Cilia dysfunction impairs the lungs’ clearing mechanism, leading to breathlessness.
- Hearing difficulties: Recurrent ear infections, owing to poor mucus clearance, can lead to hearing impairments.
- Sinusitis: Chronic sinus infections are common due to mucus congestion in the nasal passages.
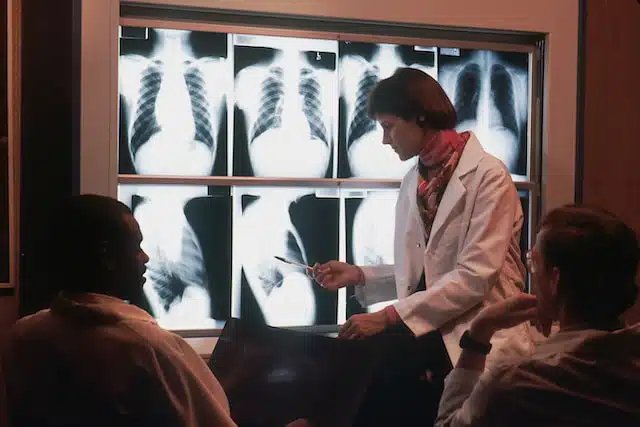
How is PCD Diagnosed?
In the realm of medical science, proper diagnosis stands as the cornerstone for effective treatment. In the case of Primary Ciliary Dyskinesia (PCD), diagnosing can be tricky due to the overlap of its symptoms with other conditions. Here, we’ll dive deep into the diagnostic tools and procedures specific to PCD, offering insights into how medical professionals determine the presence of this rare genetic condition.
Clinical Symptoms and Initial Assessment
Before venturing into specialized tests, clinicians usually perform a thorough assessment based on:
History of symptoms: Chronic respiratory infections from a young age, nasal congestion, and other recurrent symptoms might raise the suspicion of PCD.
Family history: PCD is a genetic disorder. Knowing if there are other family members diagnosed with PCD can offer significant clues.
Specialised Diagnostic Tests
Once PCD becomes a potential candidate based on initial assessments, specialized tests are employed to confirm the diagnosis.
Measurement of Nasal Nitric Oxide (nNO)
What it is: Nasal Nitric Oxide is a quick, non-invasive test that measures the levels of nitric oxide in the nasal passages.
Why it matters: People with PCD produce significantly lower amounts of nitric oxide in their nasal and sinus passages. Thus, an unusually low nNO level can be a strong indication of PCD.
Electron Microscopy
What it is: Electron Microscopy uses a specialized microscope to obtain high-resolution images of cells, revealing the ultrastructural details of cilia.
Why it matters: This method can detect abnormalities in the structure of the cilia, which are often present in PCD patients. While very detailed, it might sometimes miss certain ultrastructural defects.
Immunofluorescence Labeling
What it is: Immunofluorescence is a technique that uses specific antibodies labeled with fluorescent dyes to target particular proteins or structures in tissue samples.
Why it matters: For PCD diagnosis, it’s utilized to observe specific ciliary proteins. Abnormalities or absences in these proteins’ patterns can hint at PCD.
High-Speed Video Microscopy
What it is: This technique captures the movement of cilia in real-time, allowing for the observation of ciliary beat frequency and pattern.
Why it matters: PCD often results in an abnormal ciliary beat pattern or even immotile cilia. Observing these anomalies helps in the diagnostic process.
Genetic Testing
Given that PCD is a genetic disorder, DNA tests can be a direct approach to diagnosis:
Identifying known mutations: There are known gene mutations associated with PCD. By analyzing an individual’s genome, these mutations can be identified, confirming the diagnosis.
Predicting risk: If a person is found to carry mutations associated with PCD, genetic counseling can determine the risk of their offspring inheriting the condition.
Genetics of Primary Ciliary Dyskinesia
Primary Ciliary Dyskinesia (PCD) is not merely a condition that affects the respiratory and reproductive systems; it is deeply rooted in one’s genetic makeup. The genetic underpinnings of PCD provide insights not only into the condition itself but also into the broader realm of genetic diseases. Let’s delve into the intricate genetic landscape of PCD.
Genetic Basis of PCD
At its core, PCD is a genetic disorder, which means the condition is caused by mutations in genes essential for the proper formation and function of cilia. Cilia, the hair-like structures lining various parts of our body, particularly the respiratory tract, rely on a complex machinery of proteins for their function. A defect in any of these proteins can lead to PCD.
Key Genes and Mutations
Over 40 genes have been associated with PCD, and each of these genes encodes for a protein vital for ciliary structure or function. Some of the key genes implicated in PCD include:
DNAI1 and DNAH5: Mutations in these genes often result in the absence of the outer dynein arms, structures essential for ciliary movement.
CCDC40 and CCDC39: These genes are essential for the assembly of both inner and outer dynein arms.
RSPH1, RSPH4A, and RSPH9: Mutations here often lead to defects in the central apparatus of cilia, another component crucial for motion.
It’s essential to understand that the genetics of PCD is immensely diverse. An individual’s specific symptoms and disease severity can vary based on which gene is affected and the nature of the mutation.
Inheritance Pattern: Autosomal Recessive
PCD follows an autosomal recessive inheritance pattern. Here’s what this means:
Both copies of the gene in question (one from each parent) must have mutations for a person to have PCD. If only one copy has a mutation, the individual is a carrier but typically doesn’t show symptoms of the disease.
Carriers have a risk of passing the mutated gene to their offspring. If two carriers have a child, there’s a 25% chance the child will have PCD (by inheriting two mutated copies), a 50% chance the child will be a carrier like the parents, and a 25% chance the child will inherit two normal copies of the gene.
The Role of Genetic Testing
With advancements in genetic technologies, it’s now possible to identify PCD mutations more efficiently:
Diagnostic Aid: If PCD is suspected based on clinical symptoms, genetic testing can confirm the diagnosis by identifying mutations in known PCD genes.
Carrier Testing: For individuals with a family history of PCD, genetic tests can identify if they are carriers, helping them make informed family planning decisions.
Prenatal Testing: If both parents are known carriers of PCD mutations, prenatal tests can determine if the fetus has PCD.
Future Directions in PCD Genetics
As we continue to unravel the human genome, new genes associated with PCD might be discovered. Moreover, understanding the interplay between different genes and how they contribute to the varying severities of PCD will be crucial. Such insights can lead to personalized treatment approaches based on an individual’s genetic makeup.
Kartagener’s Syndrome: A Key Subset of PCD
Amid the labyrinth of medical terminologies and conditions, certain names stand out due to their unique nature and clinical implications. One such term intertwined with the narrative of Primary Ciliary Dyskinesia (PCD) is Kartagener’s Syndrome. Here, we’ll provide an encompassing view of this intriguing subset of PCD.
What is Kartagener’s Syndrome?
Kartagener’s Syndrome (KS) represents a specific subtype of Primary Ciliary Dyskinesia. It’s an inherited condition distinguished by a classic triad of clinical features:
Bronchiectasis: Chronic and permanent enlargement of parts of the airways of the lung, leading to frequent infections.
Sinusitis: Chronic inflammation and infection of the sinuses.
Situs inversus totalis: A congenital condition where the placement of the major visceral organs is opposite to the usual arrangement. For example, the heart might be on the right side of the chest instead of the left.
The Connection to Cilia
The reason individuals with Kartagener’s Syndrome experience these symptoms traces back to the primary defect seen in PCD: the malfunctioning cilia. These tiny hair-like structures, responsible for moving mucus and particles out of the respiratory tract, are dysfunctional in those with KS. This leads to recurrent respiratory infections (bronchiectasis and sinusitis).
The situs inversus component is a fascinating manifestation of the ciliary dysfunction. Cilia play a role in determining the positioning of organs during embryonic development. When they’re not functioning correctly, they can result in the mirrored placement of organs.
PCD and Its Impact on Fertility: A Comprehensive Look
When it comes to Primary Ciliary Dyskinesia (PCD), the conversation often revolves around the respiratory and auditory impacts. However, an equally significant, yet less discussed implication is its influence on fertility. Let’s delve into how PCD affects both male and female reproductive capabilities.
The Common Link: Cilia and Flagella
The root of PCD’s influence on fertility can be traced back to the structural and functional similarities between cilia (affected in PCD) and flagella, the tail-like structures on sperm cells. Both these structures rely on a coordinated, wave-like movement to fulfill their roles: cilia to move mucus and flagella to propel sperm. When there’s a dysfunction in cilia due to PCD, flagella often face the same fate.
Impact on Male Fertility
- Immotile or Dysfunctional Sperm
Given the shared structural similarities between cilia and flagella, men with PCD often produce sperm with flagella that are either immotile (they don’t move) or dysfunctional (they don’t move correctly). This significantly hampers the sperm’s ability to navigate through the female reproductive tract and reach the egg, leading to challenges in natural conception. - Situs Inversus and Testicular Position
Approximately half of the individuals with PCD have a condition called situs inversus, where the internal organs are mirror-reversed. Though this doesn’t directly influence sperm production, there can sometimes be associated testicular malposition, which could have implications for fertility.
Impact on Female Fertility
- Fallopian Tube Dysfunction
Cilia also line the fallopian tubes in females. These cilia play a pivotal role in guiding the egg from the ovaries to the uterus. In women with PCD, dysfunctional cilia can hinder this transportation process. If an egg cannot smoothly traverse the fallopian tubes, it may not meet the sperm, making natural conception challenging. - Increased Risk of Ectopic Pregnancies
Because of the impaired movement of the egg due to ciliary dysfunction, there’s a heightened risk for ectopic pregnancies among women with PCD. An ectopic pregnancy occurs when a fertilized egg implants and grows outside the main cavity of the uterus, most often in the fallopian tube. This is a serious and potentially life-threatening condition that requires immediate attention.
Navigating Fertility Challenges: Modern Solutions
While PCD can pose significant hurdles to natural conception, it doesn’t spell the end of parenthood dreams.
Assisted Reproductive Techniques (ART): Techniques like Intrauterine Insemination (IUI) or In-Vitro Fertilization (IVF) can be beneficial. In cases of male infertility due to PCD, techniques such as Intracytoplasmic Sperm Injection (ICSI), where a single sperm is injected directly into an egg, can be particularly effective.
Egg and Sperm Donors: For those who face significant challenges, using egg or sperm donors might be a viable option to consider.
Counseling and Support: Infertility can take an emotional toll. Engaging in counseling or joining support groups can offer emotional relief and guidance. Sharing experiences and strategies with others who’ve navigated similar challenges can be incredibly valuable.
Management of Primary Ciliary Dyskinesia
Managing Primary Ciliary Dyskinesia (PCD) demands a multifaceted approach. Given its systemic manifestations, it’s crucial to address not just the root genetic cause, but the myriad symptoms and associated conditions it spawns, particularly bronchiectasis and chronic rhinosinusitis. Let’s look at treatment strategies for these predominant manifestations of PCD.
Management of Bronchiectasis
Given the pivotal role of cilia in clearing mucus from the respiratory tract, bronchiectasis emerges as a significant concern for those with PCD. Addressing it effectively is crucial for enhancing the quality of life and prolonging longevity.
Airway Clearance: Techniques like postural drainage, chest percussion, and high-frequency chest wall oscillation devices help in loosening and clearing thickened mucus. Breathing exercises are also valuable.
Pharmacological Interventions:
Bronchodilators can help open up constricted airways, improving airflow
Mucolytics like N-acetylcysteine can thin out thick mucus, aiding in its clearance.
Antibiotics are essential for treating and sometimes preventing recurrent bacterial infections. Long-term or rotating antibiotic regimens might be prescribed for some individuals.
Anti-inflammatory agents, including corticosteroids, can help manage chronic inflammation in the airways.
Pulmonary Rehabilitation: Tailored exercise programs designed for individuals with chronic lung conditions can improve endurance, muscle strength, and overall quality of life.
Regular Monitoring: Periodic lung function tests, sputum cultures, and imaging help in monitoring the progression of bronchiectasis and guiding treatment alterations.
Managing Chronic Rhinosinusitis
Rhinosinusitis is an inflammation of the sinuses and nasal cavity, and in PCD, it’s often chronic. Effective management reduces discomfort and potential complications.
Nasal Irrigation: Regularly flushing the nasal passages with saline solutions can help in removing mucus and pathogens, reducing inflammation.
Nasal Steroids: Topical nasal corticosteroids can reduce nasal inflammation, improving breathing and reducing symptoms like nasal congestion.
Antibiotics: In the case of bacterial sinus infections, a course of antibiotics is essential.
Surgery: In severe cases, where medical management isn’t effective, surgery might be considered to widen the sinus openings and improve drainage.
Addressing Other PCD Manifestations
Apart from the primary concerns of bronchiectasis and rhinosinusitis, PCD has other potential implications that require attention:
Hearing Impairments: Regular audiometric evaluations can detect hearing loss early. Hearing aids or other interventions can be employed as necessary.
Fertility Concerns: Given the ciliary role in reproductive processes, fertility counseling and interventions might be necessary for those wanting to conceive.
Psychosocial Support: Living with a chronic condition can be mentally taxing. Support groups, counseling, and therapy can offer emotional relief and coping strategies.
Nutritional Support: Given the increased energy demands and potential for reduced appetite, nutritional counseling can ensure that individuals with PCD maintain a healthy weight and get the necessary nutrients.
Living with PCD
Daily Life Challenges
Everyday activities like climbing stairs or playing sports might be challenging. Adhering to treatments, frequent doctor visits, and managing symptoms become part and parcel of life.
Support Systems
Emotional and practical support, whether from loved ones, therapists, or support groups, can be game-changers. Sharing experiences, tips, and simply having someone who understands can make a world of difference.
Conclusion
PCD, while multifaceted and challenging, doesn’t define an individual. With advancing research, better treatment options, and growing community support, individuals with PCD are leading fulfilling, active lives.
FAQs
- What are the early signs of Primary Ciliary Dyskinesia?
- Early signs of PCD often manifest shortly after birth. They include neonatal respiratory distress, chronic cough, frequent lung and sinus infections, and recurrent ear infections leading to hearing challenges.
- Is Primary Ciliary Dyskinesia the same as Kartagener’s syndrome?
- Not exactly. Kartagener’s syndrome is a subset of PCD. Patients with Kartagener’s not only have PCD symptoms but also exhibit a unique condition called situs inversus, where internal organs are mirror-reversed from their usual positions.
- How is PCD diagnosed in children and adults?
- PCD diagnosis involves multiple tests including reduced nasal nitric oxide levels, electron microscopy to view cilia structure, immunofluorescence to identify cilia proteins, and light video microscopy to observe cilia movement.
- Can someone with PCD have children? What are the fertility implications?
- Yes, many individuals with PCD can have children. However, fertility can be a challenge. Male patients might experience immotile sperm due to flagella issues, and females might face problems due to cilia dysfunction in the fallopian tubes. Consulting a fertility specialist can provide tailored guidance.
- What is the life expectancy of someone with Primary Ciliary Dyskinesia?
- With early diagnosis, regular medical check-ups, and appropriate management, many individuals with PCD lead full, healthy lives. However, the condition requires ongoing medical attention to prevent and manage respiratory complications that could impact longevity.
- Are there any natural remedies or lifestyle changes recommended for PCD patients?
- While medical interventions are primary in PCD management, lifestyle changes like maintaining a healthy diet, staying hydrated, practicing pulmonary hygiene, avoiding smoking or second-hand smoke, and staying updated with vaccinations can be beneficial. It’s essential to consult a doctor before starting any natural remedies.
- How can I join a support group or community for PCD patients and families?
- There are numerous national and international organisations dedicated to PCD. These groups offer resources, patient experiences, and community meet-ups. Websites, social media platforms, and local hospitals can be a good starting point to find a group that resonates with your needs.
GET IN TOUCH
Schedule a Visit with Dr Ricardo Jose
Disclaimer: The information provided in this article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your healthcare provider with any questions you may have regarding a medical condition or treatment

