Living with bronchiectasis can be challenging, especially when other conditions such as asthma, COPD, GERD, chronic rhinosinusitis, rheumatoid arthritis, allergic bronchopulmonary aspergillosis (ABPA), or nontuberculous mycobacterial (NTM) lung disease are also present. These co-morbidities often overlap in symptoms and complicate both diagnosis and treatment.
This guide looks at the latest evidence-based strategies for managing these complex conditions and offers practical tips for improving daily life.
Understanding Bronchiectasis and Its Common Co-Morbidities
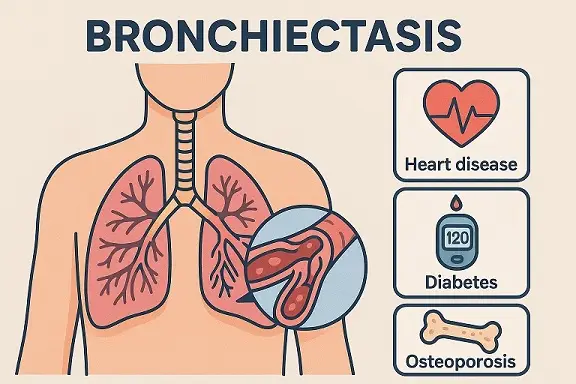
Bronchiectasis is a long-term lung disease in which the airways (bronchi) become abnormally widened. This makes it harder to clear mucus, leading to persistent infections and inflammation.
Common Co-Morbidities
- Asthma – causes airway inflammation and hyperreactivity, often co-existing with bronchiectasis in adults.
- COPD (Chronic Obstructive Pulmonary Disease) – shares symptoms such as cough, breathlessness, and sputum production.
- GERD (Gastroesophageal Reflux Disease) – acid reflux can worsen respiratory symptoms and may trigger exacerbations, or result in aspiration-related infections.
- Chronic Rhinosinusitis – upper airway inflammation often mirrors lower airway disease, contributing to a “united airways” concept. Micro-aspiration of post-nasal drip can also be a source of lower respiratory tract infections.
- ABPA – a hypersensitive reaction to Aspergillus fungi; causes inflammation and bronchial damage, resulting in bronchiectasis progression.
- NTM Lung Disease – infections by non-tuberculous mycobacteria, increasingly common in bronchiectasis patients, exacerbating symptoms.
The Overlap: A Clinical Challenge
Multiple studies highlight how co-morbid conditions can intensify disease severity. More than 50% of bronchiectasis patients have at least one coexisting airway condition. These overlaps increase hospitalisations, treatment burden, and reduce quality of life.
Shared Symptoms
- Chronic cough
- Excessive sputum production
- Wheezing or breathlessness
- Fatigue
- Recurrent chest infections
These overlaps often make accurate diagnosis and personalised treatment plans essential.
Evidence-Based Treatment Strategies
1. Airway Clearance Techniques
Essential for all patients. This includes:
- Daily physiotherapy using devices (e.g., Flutter, Acapella)
- Postural drainage
- Active cycle of breathing technique (ACBT)
- Nebulised saline (0.9–7%) to thin mucus
2. Inhaled Therapies
For asthma or COPD overlap:
- Bronchodilators (short-acting and long-acting)
- Inhaled corticosteroids (ICS) – only where eosinophilia or asthma is confirmed
3. Antibiotic Management
- Macrolides (e.g., azithromycin) – offer anti-inflammatory benefits and reduce exacerbation frequency
- Targeted oral or IV antibiotics – based on sputum culture
- Inhaled antibiotics – for Pseudomonas or other chronic infection
4. Treating ABPA
- High dose inhaled corticosteroids remain the first-line treatment.
- Oral corticosteroids are helpful to manage exacerbations.
- Itraconazole or Voriconazole – antifungal therapy in resistant cases.
- Monitor IgE levels to assess response and consider anti-IgE or anti-IL5 therapy in refractory cases.
5. Managing NTM Infections
- Long-term multidrug therapy (macrolide, rifampicin, ethambutol)
- Consider nebulised amikacin where appropraite.
- Pulsed doses of IV amikacin can also be considered where there is lack of improvement.
6. Treating rheumatoid arthiritis
- Ensuring good control of the arthritis to improve quality of life
- Balancing the benefits versus risks of immunosuppression
7. Addressing GERD and Rhinosinusitis
- GERD: Use proton pump inhibitors (PPIs), lifestyle modifications (elevated head at night, avoiding meals before bed).
- Rhinosinusitis: Nasal corticosteroids, saline irrigation, or surgery in severe cases.
Practical Tips for Patients Managing Multiple Conditions
1. Create a Symptom Diary
Track changes in symptoms, sputum colour, or breathing. Share this with your care team for better medication adjustments.
2. Stay on a Structured Airway Clearance Routine
Make physiotherapy part of your daily routine. Combine it with nebulisers if prescribed.
3. Know Your Inhalers and When to Use Them
If you have asthma or COPD overlap, ensure you understand how and when to use preventers versus relievers.
4. Get Vaccinated
Annual flu vaccines and pneumococcal vaccines help prevent severe infections.
5. Stay Hydrated and Eat Well
Mucus clears more easily when you’re hydrated. A balanced diet helps keep your immune system strong.
6. Avoid Triggers
Identify and avoid allergens, pollutants, or foods that worsen reflux or respiratory symptoms.
7. Join a Support Group
Sharing experiences can improve emotional health and offer new practical strategies.
8. Regular Check-Ups and Pulmonary Rehab
Work closely with your doctor and attend pulmonary rehabilitation if offered. It can improve exercise capacity and reduce hospital admissions.
Living Well Despite the Complexity of Bronchiectasis and Co-morbidities
While living with bronchiectasis and co-morbidities can feel overwhelming, many patients live full lives with the right management. Early diagnosis, combined with a personalised care plan and a proactive approach to daily care, makes a significant difference.
GET IN TOUCH
Schedule a Visit with Dr Jose
A Leading Bronchiectasis Specialist
Disclaimer: The information provided in this article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment, and is not an advertisement for medical products. Always seek the advice of your healthcare provider with any questions you may have regarding a medical condition or treatment. Your healthcare professional can assess your individual circumstances.
