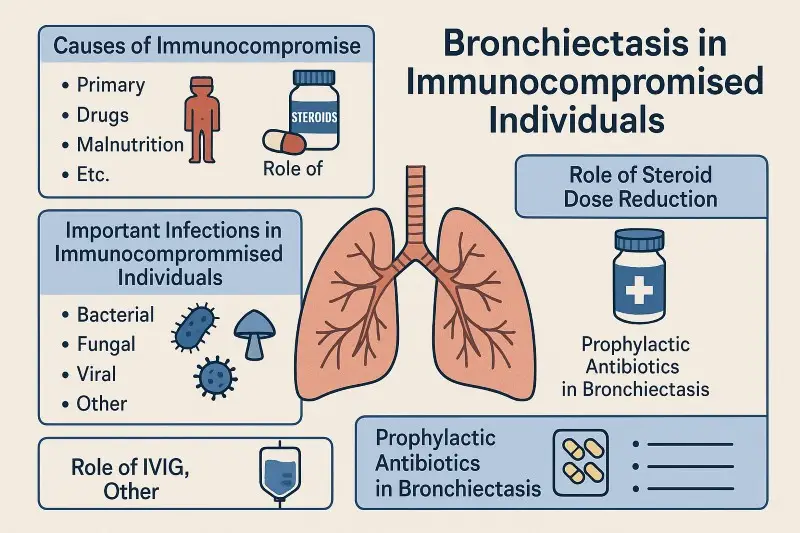
Bronchiectasis in immunocompromised individuals is a serious health issue. It develops when the airways become permanently widened and scarred after repeated infections. This lung damage makes it harder to clear mucus, leading to even more infections. The result is a vicious cycle of illness that can seriously reduce quality of life.
Understanding why immunocompromised people are at greater risk, and how treatments such as steroid dose reduction, immunoglobulin replacement, and prophylactic antibiotics can help, is key to preventing further lung injury.
What Does Immunocompromised Mean?
Being immunocompromised means the body’s defences against infection do not work as they should. This can happen for several reasons:
- Primary immunodeficiency: Genetic conditions such as common variable immunodeficiency (CVID), X-linked agammaglobulinaemia (XLA), and IgG subclass deficiency. These conditions reduce or prevent the production of antibodies, which are essential for fighting infection.
- Secondary immunodeficiency: This is more common and can be caused by:
- Long-term steroid use or immunosuppressive drugs for conditions such as autoimmune disease or after transplant.
- HIV infection, which damages the immune system directly.
- Cancers of the blood, such as leukaemia or myeloma.
- Severe malnutrition, which weakens the whole immune response.
- Older age, which naturally reduces immune function.
All of these conditions make the lungs more vulnerable to infections. Repeated chest infections over time can lead to bronchiectasis.
Why Bronchiectasis Develops in Immunocompromised People
When the immune system cannot fight off infections, bacteria, viruses, and fungi remain in the airways longer. Mucus builds up, inflammation increases, and the airway walls become damaged. The airways widen permanently and lose their ability to clear mucus effectively. This leads to more infections and more damage. In immunocompromised individuals, this process can move faster and be harder to control.
Infections That Commonly Affect the Lungs in Immunocompromised People
Immunocompromised individuals face a wider range of infections than the general population. These include:
- Bacterial infections: The most common bacteria are Haemophilus influenzae and Streptococcus pneumoniae. Chronic colonisation with Pseudomonas aeruginosa is particularly harmful. Once Pseudomonas settles in the lungs, it is very difficult to eradicate and it speeds up the decline in lung function.
- Non-tuberculous mycobacteria (NTM): These are harder to treat than common bacteria and often require long courses of antibiotics.
- Fungal infections: Aspergillus can infect the lungs directly or cause allergic bronchopulmonary aspergillosis (ABPA), a severe allergic reaction that damages the airways.
- Viral infections: Influenza, RSV, and COVID-19 are well known for triggering exacerbations of bronchiectasis. In HIV or patients with very weak immunity, viruses like CMV can also play a role.
- Opportunistic infections: In severely immunocompromised people, unusual organisms such as Pneumocystis jirovecii or Nocardia can cause pneumonia.
Knowing which infection is present is vital because treatment varies for each type.
The Role of Steroid Dose Reduction
Steroids such as prednisolone are powerful drugs that reduce inflammation and control many diseases. Unfortunately, they also weaken the immune system. The higher the dose and the longer the treatment, the greater the risk of infections.
For patients with bronchiectasis, this creates a difficult balance. Steroids may be needed to treat asthma, allergic bronchopulmonary aspergillosis, or autoimmune disease, but they also make the lungs more vulnerable.
The recommendation is to reduce doses of steroids to the lowest possible dose that still controls the underlying condition. For example, doses below 5–10 mg of prednisolone daily are far less likely to cause significant immune suppression than higher doses. Reducing steroid exposure helps the immune system fight off infections and lowers the risk of further airway damage.
The Role of Immunoglobulin Replacement (IVIG and SCIG)
Some people with bronchiectasis are immunocompromised because their body cannot make enough antibodies. This is common in conditions such as CVID or XLA. For these patients, immunoglobulin replacement therapy is lifesaving.
Immunoglobulin can be given through a vein (IVIG) every 3–4 weeks or under the skin (SCIG) weekly. It supplies the body with ready-made antibodies to fight infections. Patients on immunoglobulin therapy have fewer chest infections, fewer hospital visits, and slower progression of lung disease.
For people with bronchiectasis, respiratory immunologists often aim for higher antibody levels than usual. This is because lung disease increases the body’s use of antibodies. Standard doses are around 0.4–0.6 g per kilogram of body weight each month, but this may be increased to achieve protective levels.
Some studies suggest that in stable patients without lung disease, the dose of immunoglobulin can sometimes be reduced. However, in patients with bronchiectasis, full dosing is usually needed. Skipping or lowering the dose can increase infection risk and lead to further lung damage.
Prophylactic Antibiotics in Bronchiectasis in Immunocompromised individuals.
Antibiotics are not just for treating infections. In some cases, they can also be used long-term to prevent them. This approach is called antibiotic prophylaxis.
When Doctors Recommend Prophylactic Antibiotics
- If a person has three or more exacerbations per year.
- If Pseudomonas aeruginosa is found in sputum samples.
- If patients remain unwell despite airway clearance and immunoglobulin therapy.
- If infections keep leading to hospital admissions.
Types of Prophylactic Antibiotics
Macrolides are the most common choice. Azithromycin (e.g. 250 mg daily or three times a week) and erythromycin have been shown to reduce exacerbations. They also reduce airway inflammation. People need an ECG before starting to check the heart rhythm and a sputum test for non-tuberculous mycobacteria.
Inhaled antibiotics are often used when Pseudomonas is present. Drugs such as inhaled tobramycin, colistin, or gentamicin are delivered directly into the lungs through a nebuliser. This reduces bacterial load in the airways and helps prevent flare-ups.
Other prophylaxis may be needed for very immunocompromised patients. For example, co-trimoxazole is used to prevent Pneumocystis jirovecii pneumonia in patients on high-dose steroids, chemotherapy, or with advanced HIV.
Important Point
Prophylactic antibiotics are not a cure. They reduce but do not eliminate the risk of infection. Treatment must be reviewed every 6–12 months to check if it is still effective, whether resistance has developed, and whether side effects are occurring. They should always be combined with airway clearance, immunoglobulin therapy (if needed), and vaccinations.
A Comprehensive Management Plan
Managing bronchiectasis in immunocompromised individuals requires a team approach. Key steps include:
- Early diagnosis: High-resolution CT scans and lung function tests can detect bronchiectasis before it causes severe damage.
- Optimising immunity: Immunoglobulin replacement for antibody deficiency, tapering steroids to the lowest dose, and avoiding unnecessary immunosuppressants.
- Preventing infections: Vaccinations, prophylactic antibiotics when indicated, and prompt treatment of chest infections.
- Airway clearance: Daily physiotherapy, devices to help remove mucus, and exercise.
- Nutrition support: Good diet and supplements if malnutrition is present.
- Regular monitoring: Sputum cultures, lung function, and imaging to track disease progression.
- Specialist input: Care from respiratory infection specialists, immunologists, and physiotherapists for best results.
Conclusion
Bronchiectasis in immunocompromised individuals is a challenging condition, but it can be managed effectively. Reducing steroid doses, optimising immunoglobulin replacement, and using prophylactic antibiotics all play a central role. With early recognition, careful monitoring, and a personalised treatment plan, many patients can avoid repeated infections, protect their lung function, and enjoy a better quality of life.
Frequently Asked Questions (FAQs)
Can bronchiectasis be cured?
No. Bronchiectasis is a permanent change in the airways. However, with good treatment, infections can be reduced, symptoms can improve, and the disease can be stabilised.
Is immunoglobulin replacement safe long term?
Yes. IVIG and SCIG have been used safely for decades. Side effects are usually mild, such as headache or tiredness after an infusion. Severe side effects are very rare. The benefits of preventing infections far outweigh the risks.
Do prophylactic antibiotics cause resistance?
There is a risk of resistance, which is why doctors review the treatment regularly. The benefits of fewer infections usually outweigh the risks, especially in people with frequent flare-ups. Careful monitoring helps to minimise problems.
Why do doctors want to reduce steroid doses?
Steroids can save lives, but they weaken the immune system. Lowering the dose helps the immune system fight infections more effectively. Reducing steroids also lowers the risk of long-term side effects like osteoporosis, diabetes, and high blood pressure.
What can patients do at home to help?
Daily airway clearance exercises, keeping up with vaccinations, eating a balanced diet, staying active, and reporting infections early all make a big difference. Working closely with the healthcare team helps keep the condition under control.
GET IN TOUCH
Schedule a Visit with Dr Ricardo Jose
Disclaimer: The information provided in this article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your healthcare provider with any questions you may have regarding a medical condition or treatment
