The world of respiratory health presents many challenges, and this includes the complications of bronchiectasis. Bronchiectasis is a condition, characterised by the permanent enlargement of the bronchial tubes, and is often debilitating. This blog highlights some of the important complications of bronchiectasis, with a focus on bacterial colonisation, frequent exacerbations, non-tuberculous mycobacteria (NTM) infections, fungal diseases like chronic pulmonary aspergillosis, cardiovascular implications, and respiratory failure.
Bacterial Colonisation and Frequent Exacerbations in Bronchiectasis
Bronchiectasis creates a lung environment ripe for bacterial colonisation. The abnormal dilation of the bronchial tubes encourages mucus accumulation, a prime breeding ground for bacteria. This can lead to frequent exacerbations, characterised by an intense flare-up of symptoms that may persist for days.
Understanding the specific bacterial colonisation and the severity of the infection can guide personalised treatment plans to mitigate these exacerbations.
Bronchiectasis and Non-Tuberculous Mycobacteria Infections
Bronchiectasis patients can also be prone to non-tuberculous mycobacteria (NTM) infections. NTMs are bacteria found in soil and water, and people with bronchiectasis are susceptible due to changes in their lung structure. The ensuing infections can further deteriorate lung function, causing additional symptoms that compound the effects of bronchiectasis.
Bronchiectasis and Fungal Diseases
Fungal diseases such as Chronic Pulmonary Aspergillosis (CPA) often intertwine with bronchiectasis. CPA is a long-term fungal infection triggered by Aspergillus species, and it commonly affects individuals with pre-existing lung conditions like bronchiectasis. Symptoms of CPA, such as persistent cough, fatigue, and weight loss, can intensify the bronchiectasis condition, posing management challenges.
The Cardiovascular Complications of Bronchiectasis
Bronchiectasis also brings cardiovascular complications into the picture.
One primary complication is cor pulmonale, a condition characterised by alteration of the structure and function of the right ventricle of the heart as a direct result of a respiratory disorder. Prolonged bronchiectasis can cause chronic hypoxia, leading to pulmonary hypertension. Over time, this increased pressure in the pulmonary arteries adds a strain on the right ventricle, which can lead to cor pulmonale.
Apart from cor pulmonale, bronchiectasis patients also face an elevated risk of experiencing other cardiovascular events, including heart failure, stroke, and arrhythmias. Frequent exacerbations common in bronchiectasis can lead to systemic inflammation, which has been linked to atherosclerosis, a condition where the arteries narrow and harden due to plaque build-up. This can further escalate the risk of acute cardiovascular events.
Bronchiectasis can also be associated with venous thromboembolism (VTE), a condition where a blood clot forms in the deep veins of the body, often in the legs, and can travel to the lungs, causing a life-threatening condition called pulmonary embolism.
Recognising these potential cardiovascular complications in bronchiectasis patients is paramount for providing comprehensive care. Early detection and proactive management can significantly reduce cardiovascular morbidity and mortality in these individuals.
Respiratory specialists with an interest in bronchiectasis must take an integrative approach towards patient management, considering both the respiratory and cardiovascular aspects of bronchiectasis. Regular cardiovascular assessments and close monitoring can help identify early signs of cardiac issues. At the same time, optimising bronchiectasis management, including effective control of exacerbations and maintaining optimal lung function, can help reduce the risk of cardiovascular complications.
Respiratory Failure: The Severe End-Stage of Bronchiectasis
Respiratory failure represents one of the most severe complications of bronchiectasis, manifesting when the lungs can no longer efficiently exchange gases. In this dire situation, patients’ blood may not receive sufficient oxygen, or it may struggle to eliminate carbon dioxide effectively, leading to life-threatening consequences.
In bronchiectasis, respiratory failure can occur due to several factors. The recurrent infections and inflammation associated with the condition can progressively damage the lung tissue, leading to a loss of functional alveoli – the tiny air sacs responsible for oxygen-carbon dioxide exchange. This, in turn, compromises the lungs’ ability to oxygenate the blood and remove carbon dioxide.
Patients experiencing respiratory failure may present with symptoms like shortness of breath, increased heart rate, rapid breathing, confusion, and a bluish colour in the skin, lips, or fingertips. Notably, these symptoms demand immediate medical attention.
One management strategy for respiratory failure, particularly in a chronic setting, is non-invasive ventilation (NIV). NIV provides ventilatory support through the patient’s upper airway using a mask or similar device. This approach has shown promise in managing other chronic respiratory conditions like chronic obstructive pulmonary disease (COPD) and is gaining recognition for its potential benefits in bronchiectasis with centres like the Royal Brompton Hospital in London having extensive experience of the use of NIV in bronchiectasis.
NIV in bronchiectasis works by assisting the compromised respiratory muscles, improving the efficiency of gas exchange, and helping clear the airways of excess mucus. It can offer relief from symptoms, enhance quality of life, and reduce the frequency of hospital admissions.
However, the use of NIV in bronchiectasis is not without its challenges. It requires careful patient selection, close monitoring, and adjustments to ensure the comfort and compliance of the patient. The long-term benefits and potential risks of NIV in bronchiectasis are still being investigated, highlighting the need for further high-quality research.
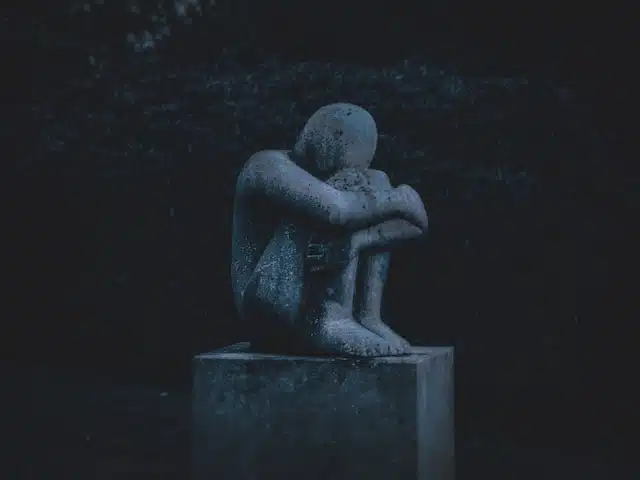
The Psychological Impact of Bronchiectasis
Lastly, let’s not overlook the psychological implications of living with bronchiectasis.
While the physical toll of bronchiectasis is widely recognised, the psychological impact of the disease often remains overlooked. Yet, the mental health aspect is crucial, with a significant proportion of bronchiectasis patients reporting symptoms of anxiety, depression, and reduced quality of life.
Living with a chronic illness such as bronchiectasis can be mentally and emotionally draining. Frequent cough, breathlessness, fatigue and recurrent infections, which are characteristic symptoms of bronchiectasis, can profoundly affect daily life and personal independence. This can lead to feelings of frustration, fear, and social isolation.
Moreover, the unpredictability of exacerbations adds an element of anxiety and stress. The fear of an impending flare-up can lead to heightened worry and constant vigilance, affecting emotional well-being and mental peace.
Depression is another significant concern among bronchiectasis patients. The constant battle with ill health, coupled with a possible reduction in social activities due to physical limitations, can foster feelings of hopelessness and sadness. If left unaddressed, these can escalate into clinical depression.
The potential stigma attached to a chronic cough or breathlessness can also affect a patient’s self-esteem and social interactions, further exacerbating feelings of isolation and anxiety.
Recognising and addressing these psychological impacts is a crucial part of comprehensive bronchiectasis care. A multidisciplinary approach that includes psychologists and counsellors, alongside respiratory specialists, can help patients cope better with their condition.
Psychotherapy, including cognitive-behavioural therapy, can equip patients with skills to manage stress, anxiety and depressive symptoms. Relaxation techniques, mindfulness and regular exercise can also play a role in alleviating psychological distress.
Peer support groups, either in person or online, can provide a safe space for patients to share their experiences, learn from others and gain emotional support. Additionally, family and caregiver education about bronchiectasis can foster a more understanding and supportive home environment for patients.
If you need help for your depression please contact the Samaritans of Depression UK charities.
GET IN TOUCH
Schedule a Visit
Disclaimer: The information provided in this article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your healthcare provider with any questions you may have regarding a medical condition or treatment.

