Introduction
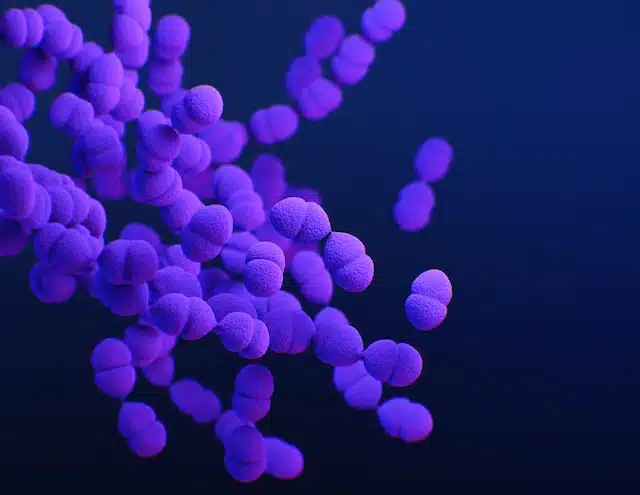
There’s a storm brewing on the horizon of healthcare, and it’s not to be taken lightly. Emerging multi-drug resistant pathogens causing pneumonia are rearing their heads, and among them, the ESKAPE group is leading the rebellion. Ready for a closer look?
The ESKAPE pathogens
Acinetobacter Pneumoniae: The Silent Usurper
Epidemiology
- Acinetobacter species, particularly A. baumannii, have become significant hospital pathogens. They’re responsible for a variety of nosocomial infections.
- Often isolated in intensive care units, this pathogen’s outbreaks have been documented worldwide.
Risks and Mortality
- Acinetobacter infections come with high mortality rates, especially ventilator-associated pneumonia.
- Resistance to first-line antibiotics has made treatment challenging, sometimes leading to dire outcomes.
Pseudomonas Aeruginosa: The Tenacious Adversary
Epidemiology
- Pseudomonas is ubiquitous in the environment but turns particularly nasty in hospital settings.
- It’s the third most common nosocomial pathogen, causing pneumonia, urinary tract infections, and sepsis.
Risks and Mortality
- Mortality rates with Pseudomonas-induced pneumonia can be alarmingly high, especially if not treated promptly.
- With its knack for biofilm formation, it’s a master of evasion, making treatment all the more complex.
Stenotrophomonas Maltophilia: The Underdog with a Punch
Epidemiology
- Previously considered a mere contaminant, its clinical significance in hospital-acquired infections has surged.
- It’s been increasingly isolated in respiratory secretions of patients with pneumonia.
Risks and Mortality
- Infections can lead to severe complications, especially in immunocompromised individuals.
- The bacteria’s intrinsic resistance to many antibiotics paints a concerning picture for patient outcomes.
Staphylococcus Aureus: The Familiar Foe
Epidemiology
- A common pathogen, it’s found in the noses of about 30% of the global population.
- MRSA (Methicillin-resistant Staphylococcus aureus), its drug-resistant variant, poses a heightened threat in healthcare facilities.
Risks and Mortality
- Staph infections can range from mild skin conditions to severe pneumonia and sepsis.
- MRSA-related pneumonia comes with a high mortality rate, especially when antibiotic intervention is delayed.
Enterococcus Faecium & Klebsiella Pneumoniae: The Dynamic Duo
Epidemiology
- Both are regulars in human guts but become problematic when they venture out.
- They’ve made their mark in healthcare settings, causing a variety of infections, including pneumonia.
Risks and Mortality
- Their drug-resistant variants, VRE (Vancomycin-resistant enterococci) and KPC (Klebsiella pneumoniae carbapenemase), respectively, are particularly worrisome.
- Associated with prolonged hospital stays, these infections often culminate in increased fatalities, given their resistance profile.
The New-age Microbial Menace
The Lowdown on These Mighty Microbes
- Adaptability is their middle name. These pathogens, not content with the usual mischief, have upped their game. They’ve developed resistance mechanisms against multiple drugs, meaning they’re no longer the pushovers they once were!
- We’ve got ourselves a mix. We’re talking about bacteria, viruses, and fungi. No stone is left unturned in their quest for domination.
- Playing hard to get. Traditional treatments? They laugh in the face of them! These resistant strains need a new kind of attention to be tackled.
Why The Fuss?
More than Just a Tough Bug
- Rising Hospital Stays: Patients are stuck in hospital rooms for longer. And, we all know, nobody likes being cooped up in there, right?
- Higher Treatment Costs: It ain’t just about the money, honey. With these bad boys on the prowl, treatments are pricier, and outcomes? Less predictable.
- Increased Mortality Rates: This one’s no joke. We’re seeing higher fatalities. Talk about a double whammy!
But How Did We Get Here?
The Road to Resistance
- Overuse and Misuse: Popping pills like candy? Big no-no. Overusing and misusing antibiotics has been a major party pooper. The bugs are getting smarter because we’re giving them a chance!
- Incomplete Courses: You remember that antibiotic course you ditched halfway because you felt better? Yup, that’s part of the problem.
- Environmental Factors: From industrial waste to animal farming, many factors play into this messy potpourri. A little bit of this, a little bit of that, and voila! Superbugs galore.
FAQs: Unraveling the Mystery
- Q: What exactly is drug resistance?A: In simple words? It’s when our micro-enemies decide that our drugs don’t scare them anymore. They develop mechanisms to defend themselves, rendering treatments ineffective.
- Q: Are these emerging multi-drug resistant pathogens causing pneumonia really that dangerous?A: Absolutely! These aren’t your garden-variety bugs. They’re more resilient, harder to treat, and can lead to more severe cases of pneumonia.
- Q: How can I protect myself and my family?A: Great question! Stick to prescribed medications, complete your antibiotic courses, and promote awareness. Knowledge is power, after all!
- Q: Why are the ESKAPE pathogens particularly troublesome?
A: Their ability to swiftly develop resistance and thrive in healthcare settings makes them a formidable challenge to clinicians. - Q: Can we foresee an end to this rising threat?
A: With rigorous research, public awareness, and global collaborative efforts, we can hope to curtail their spread and impact. - Q: Is drug resistance the same for all these pathogens?
A: Not quite. Each has its own sneaky ways of dodging our drugs, which makes them uniquely challenging. - Q: How widespread is this problem?
A: More than we’d like. Many countries are reporting cases, especially in hospital settings. - Q: Any advice to keep these infections at bay?
A: Absolutely. Stick to prescribed meds, finish your courses, and keep top-notch hygiene habits. Prevention is the name of the game.
Conclusion: A Call to Arms
The emerging multi-drug resistant ESKAPE pathogens causing pneumonia are undeniably a grave concern. However, armed with knowledge and a collective will, the medical community and public at large can mount a formidable defence. Challenges are aplenty, but in the face of adversity, innovation and collaboration often shine brightest. The fight is on!
GET IN TOUCH
Schedule a Visit with Dr Ricardo Jose
Disclaimer: The information provided in this article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your healthcare provider with any questions you may have regarding a medical condition or treatment

