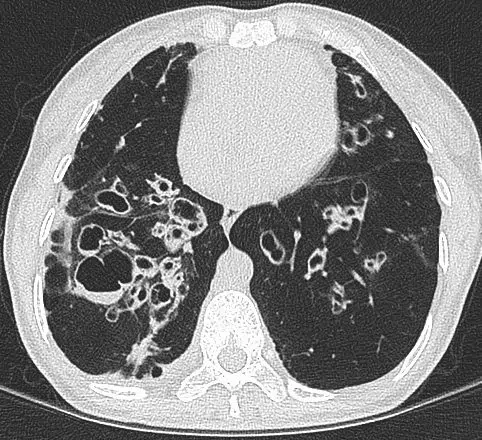
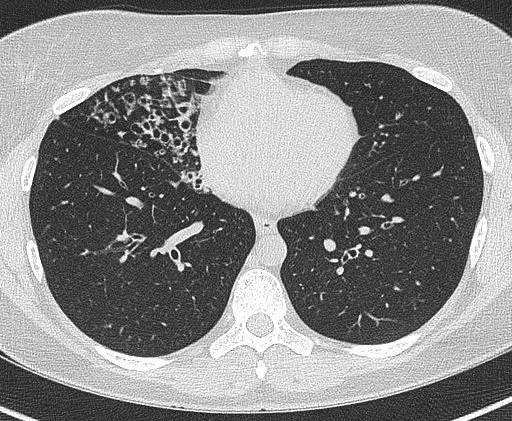
Bronchiectasis is a lung disease characterized by the permanent widening of the bronchial tubes, causing them to lose their normal shape and ability to clear mucus.
Clinically it is associated with cough, production of phlegm (mucus) and recurrent chest infection.
Bronchiectasis is a complex disease with a multifactorial pathogenesis that involves damage to the airways and an ongoing cycle of infection and inflammation.

Patients with bronchiectasis may experience a range of symptoms that affect their daily life and quality of life. Common symptoms include:
The following are some of the key steps in the development and progression of bronchiectasis:
A detailed history and examination, as well as targeted investigations can identify the cause of bronchiectasis in many cases. However, a proportion will be labelled “idiopathic” where the cause is unknown.
A mutation in the cystic fibrosis transmembrane regulator gene (CFTR) on chromosome 7 results in thick mucus that blocks ducts in various organs (e.g. lungs, pancreas, liver, intestines, cervix, vas deferens). To get the disease a person needs to acquire an abnormal gene from each parent.
The diagnosis is made from the clinical history, a chloride sweat test and genetic testing.
Treatment differs from that in non-CF bronchiectasis particularly with the novel medication (e.g. Kaftrio) for patients with specific gene mutations.
Primary Ciliary Dyskinesia (PCD) is also known as immotile cilia syndrome. It is an inherited condition associated with ciliary abnormalities. Cilia are hair-like structures attached to cells of the lining of the upper and lower respiratory tract, the eustachian tube, the cochlear in the ears and the male vas-deferens (a duct that transports sperm form the epididymus to the ejaculatory canal). When these cell don’t function normally they results in abnormal clearance of mucus in the airways and chest infections, sinus and ear infections, loss of hearing and infertility. During development of the fetus cilia are also responsible for the movement of developing organs to their correct position and half of people affected by PCD can have dextrocardia (heart on the right side of the chest) or situs inversus where all the organs are on opposite sides.
The inability to clear mucus and recurrent chest infections results in bronchiectasis.
Parts of the immune system (immune cells or antibodies) are missing or not working properly mostly due to errors in the genes. The primary immunodeficiency disorders (PID) consist of over 300 conditions with a wide spectrum of disease severity. They are usually identified in childhood but some less severe conditions are only diagnosed later in life.
The impaired immune function predispose to recurrent and severe infections that often taken longer to improve on antibiotic therapy. Infections may be due to opportunistic pathogens that are harder to diagnose.
Once there is suspicion of a PID the diagnosis is usually by specialist laboratory tests carried out by an immunologist
Alpha-1 anti-trypsin (A1AT) is a protein that neutralises various proteases (e.g. neutrophil elastase) and protects organs such as the lungs from damaged cause by these proteases. A1AT deficiency is caused by a genetic mutation in the SERPINA 1 gene resulting in low levels of A1AT. Low levels of A1AT can’t protect the lungs from damage caused by inflammation following exposure to smoke or dust, or chest infections, resulting in tissue damage. People with A1AT are more likely to develop COPD at a younger age and can develop bronchiectasis. It is very important that people with A1AT don’t smoke. Also, screening of close relatives should be undertaken to establish a diagnosis and counsel on preventing lung disease.
The immune system can be affected by disease, medication and toxins. The impaired immune system results in recurrent and severe infections that take longer to improve on antibiotics. Infections may be due to opportunistic pathogens that are harder to diagnose.
Common diseases causing secondary immunodeficiency (SID):
Common treatments causing SID:
Infections of the lungs are probably the most common cause of bronchiectasis. These may be severe infections such as pneumonia and tuberculosis, or other childhood infections that may affect the chest such measles and Whooping cough. Often by the time bronchiectasis becomes a problem in adulthood the occurrence of childhood infections is not recalled. Importantly, aspiration pneumonia is also an important cause of bronchiectasis and is often seen in patients with head and neck cancer or post-stroke.
Allergic bronchopulmonary aspergillosis (APBA) is caused by an allergic immune reaction in the airways to the mould of the Aspergillus species. A similar condition when the allergy is due to other fungi and is termed allergic bronchopulmonary mycosis (ABPM). It usually occurs in patients with asthma and causes symptoms of shortness of breath, wheeze, cough (including coughing blood), mucus production and intermittent fevers.
The diagnosis is made clinically with the support of investigations confirming sensitisation to the fungus. The pattern of flitting consolidation and bronchoceles as well as obstructive lung function tests also support the diagnosis.
Treatment involves targeting the allergic inflammation in the airways with inhaled corticosteroids, oral corticosteroids (e.g. prednisolone) and anti-fungal medications (e.g. itraconazole, voriconazole and posaconazole)
More commonly seen in children, the obstruction of an airway by a foreign object can result in distal bronchiectasis and recurrent infections. A history of aspiration (e.g. during dental treatment) is important in considering the diagnosis that may be diagnosed on radiological imaging of the chest or at bronchoscopy.
Obstruction of the airway by a tumour can also result in distal bronchiectasis.
Connective tissue disorders are those where the tissue (e.g. tendons, ligaments, cartilage, skin, eyes) containing collagen and elastin that connects different parts of the body are inflamed.
They include:
Investigations are carried out to determine the presence of specific auto-antibodies in blood to establish the presence of a CTD.
CTD is associated with bronchiectasis with the presence of bronchiectasis sometimes predating the presentation of CTD features (painful and swollen joints, rashes, etc.)
Ulcerative colitis is an inflammatory disorder of the colon that results in symptoms of loose stools, abdominal pain and bloody bowel movements. It can also cause fevers, weight loss and fatigue and be associated with joint pain. The diagnosis is made by a gastroenterologist who will do a colonsocopy and take biopsies of the lining of the colon. A test of the faeces (fecal calprotectin) if low makes the disease unlikely.
Although the mechanism of how it affects the lungs isn’t known, bronchiectasis is associated with ulcerative colitis.


Airway clearance is the mainstay of bronchiectasis management and it is importanta to get the advise of a specialist respiratory physiotherapist.
This may involve the following techniques:
Sometimes adjuncts are needed to help expectorate the phlegm including the use of an Acapella or Aerobika flutter valves or a positive expiratory pressure (PEP) valve.
Medication can also be used to help alter the viscocity of the mucus and assist with clearance. Nebulised saline (NaCl) is often used with concentrations ranging from 0.9% (isotonic) to 7% (hypertonic) as well as other mucolytics such as carbocisteine.
Videos on airway clearance techniques can be seen here.
The treatment of active chest infections and exacerbations of bronchiectasis is with antibiotics. In individuals with bronchiectasis these need to be tailored at the usual pathogens that are cultured in the sputum and for an appropriate duration (usually 10 – 14 days).
Prophylactic (preventative) antibiotics are usually prescribed when there is a history of frequent infections or exacerbations of bronchiectasis (3 or more in 12 months). depending on the individual case these may be recommended seasonally or all year round. Prophylactic antibiotics may be given orally or in some cases via the nebulised route.
Azithromycin is an antibiotic with immunomodulatory properties. In addition to its ability to stop bacteria from growing it is able to change the way the immune system functions or responds. It has been shown to reduce the frequency of bronchiectasis exacerbations in patients with Pseudmonas aeruginosa infections and to reduce phlegm volume.
It is recommended that patients with bronchiectasis receive the annual influenza (Flu) vaccination and the pneumococcal polysaccharide vaccine (PPV23) if they have low total pneumococcal or specific pneumococcal serotype antibody levels. Some times other vaccines are adminsitered as part of testing of the immune system function (e.g. tetanus vaccine).
Respiratory Medicine
Royal Brompton Hospital
Sydney Street
Chelsea
SW3 6NP